The human leukocyte antigen system (HLA) is the name of the major histocompatibility complex (MHC) in humans. The superlocus contains a large number of genes related to immune system function in humans. This group of genes reside on chromosome 6,

Chromosome 6

HLA TYPES LOCATION IN GENE 6
and encode cell-surface antigen-presenting proteins and many other genes. The HLA genes are the human versions of the MHC genes that are found in most vertebrates (and thus are the most studied of the MHC genes). The proteins encoded by certain genes are also known as antigens, as a result of their historic discovery as factors in organ transplantations. The major HLA antigens are essential elements for immune function. Different classes have different functions:
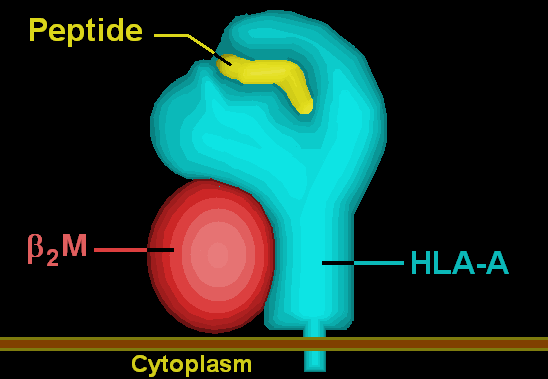
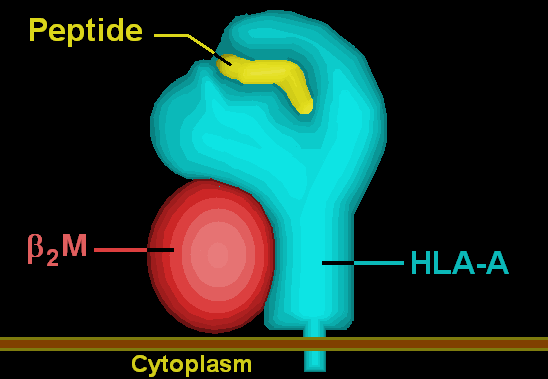
HLA class I antigens (A, B & C) present peptides from inside the cell (including viral peptides if present). These peptides are produced from digested proteins that are broken down in the proteasomes. The peptides are generally small polymers, about 9 amino acids in length. Foreign antigens attract killer T-cells (also called CD8 positive- or cytotoxic T-cells) that destroy cells.
HLA class II antigens (DP,DM, DOA,DOB,DQ, & DR) present antigens from outside of the cell to T-lymphocytes. These particular antigens stimulate T-helper cells to multiply, and these T-helper cells then stimulate antibody-producing B-cells to produce Antibodies to that specific antigen. Self-antigens are suppressed by suppressor T-cells.
HLA class III antigens encode components of the complement system.
HLA have other roles. They are important in disease defense. They may be the cause of organ transplant rejections. They may protect against or fail to protect (if down regulated by an infection) cancers. They may mediate autoimmune disease (examples: type I diabetes, coeliac disease). Also, in reproduction, HLA may be related to the individual smell of people and may be involved in mate selection .
Aside from the genes encoding the 6 major antigens, there are a large number of other genes, many involved in immune function, located on the HLA complex. Diversity of HLA in human population is one aspect of disease defense, and, as a result, the chance of two unrelated individuals having identical HLA molecules on all loci is very low. Historically, HLA genes were identified as a result of the ability to successfully transplant organs between HLA similar individuals.
Functions
The proteins encoded by HLAs are those on the outer part of body cells that are (effectively) unique to that person. The immune system uses the HLAs to differentiate self cells and non-self cells. Any cell displaying that person's HLA type belongs to that person (and therefore is not an invader).
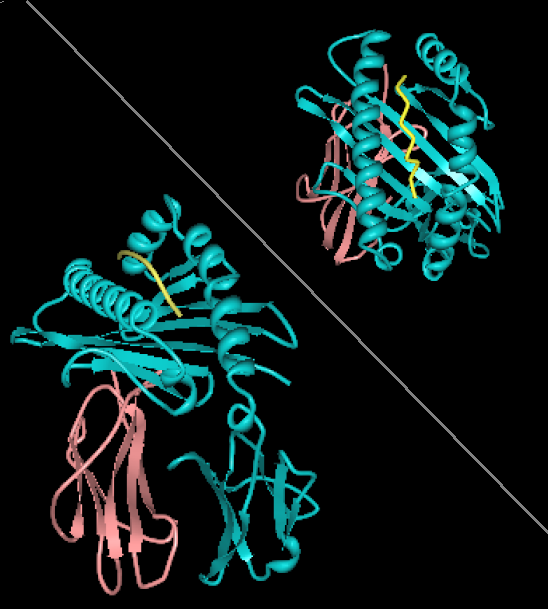
DR protein (DRA:DRB1*0101 gene products) with bound Staphylococcal enterotoxin ligand (subunit I-C), view is top down showing all DR amino acid residues within 5 Angstroms of the SEI peptide.
In infectious disease. When a foreign pathogen enters the body, specific cells called antigen-presenting cells (APCs) engulf the pathogen through a process called phagocytosis. Proteins from the pathogen are digested into small pieces (peptides) and loaded onto HLA antigens (specifically MHC class II). They are then displayed by the antigen presenting cells for certain cells of the immune system called T cells, which then produce a variety of effects to eliminate the pathogen.
Through a similar process, proteins (both native and foreign, such as the proteins of viruses) produced inside most cells are displayed on HLA antigens (specifically MHC class I) on the cell surface. Infected cells can be recognized and destroyed by components of the immune system (specifically CD8+ T cells).
The image off to the side shows a piece of a poisonous bacterial protein (SEI peptide) bound within the binding cleft portion of the HLA-DR1 molecule. In the illustration far below, a different view, one can see an entire DQ with a bound peptide in a similar cleft, as viewed from the side. Disease-related peptides fit into these 'slots' much like a hand fits into a glove or a key fits into a lock. In these configurations peptides are presented to T-cells. The T-cells are restricted by the HLA molecules when certain peptides are within the binding cleft. These cells have receptors that are like antibodies and each cell only recognizes a few class II-peptide combinations. Once a T-cell recognizes a peptide within an MHC class II molecule it can stimulate B-cells that also recognize the same molecule in their sIgM antibodies. Therefore these T-cells help B-cells make antibodies to proteins they both recognize. There are billions of different T-cells in each person that can be made to recognize antigens, many are removed because they recognize self antigens. Each HLA can bind many peptides, and each person has 3 HLA types and can have 4 isoforms of DP, 4 isoforms of DQ and 4 Isoforms of DR (2 of DRB1, and 2 of DRB3,DRB4, or DRB5) for a total of 12 isoforms. In such heterozygotes it is difficult for disease related proteins to escape detection.
In graft rejection. Any cell displaying some other HLA type is "non-self" and is an invader, resulting in the rejection of the tissue bearing those cells. Because of the importance of HLA in transplantation, the HLA loci are among of the most frequently typed by serology or PCR relative to any other autosomal alleles.
In autoimmunity. HLA types are inherited, and some of them are connected with autoimmune disorders and other diseases. People with certain HLA antigens are more likely to develop certain autoimmune diseases, such as Type I Diabetes, Ankylosing spondylitis, Celiac Disease, SLE (Systemic Lupus Erythematosus), Myasthenia Gravis, inclusion body myositis and Sjögren's syndrome. HLA typing has led to some improvement and acceleration in the diagnosis of Celiac Disease and Type 1 diabetes; however for DQ2 typing to be useful it requires either high resolution B1*typing (resolving *0201 from *0202), DQA1*typing, or DR serotyping. Current serotyping can resolve, in one step, DQ8. HLA typing in autoimmunity is being increasingly used as a tool in diagnosis. In Celiac disease it is the only effective means of discriminating between 1st degree relatives who are at risk from those who are not at risk, prior to the appearance of sometimes irreversible symptoms such as allergies and secondary autoimmune disease.
In cancer. Some HLA mediated diseases are directly involved in the promotion of cancer. Gluten sensitive enteropathy is associated with increased prevalence of Enteropathy-associated T-cell Lymphoma, and DR3-DQ2 homozygotes are within the highest risk group with close to 80% of gluten sensitive EATL cases. More often, however, HLA molecules play a protective role, recognizing the increase in antigens that were not tolerated because of low levels in the normal state. Abnormal cells may be targeted for apoptosis mediating many cancers before clinical diagnosis. Prevention of cancer may be a portion of heterozygous selection acting on HLA.
Classification
MHC class I proteins form a functional receptor on most nucleated cells of the body.
There are 3 major and 3 minor MHC class I genes in HLA:
HLA-A
HLA-A are a group of human leukocyte antigens (HLA) that are encoded by the HLA-A locus on human chromosome 6p. The HLA genes constitute a large subset of the Major histocompatibility complex (MHC) of humans. HLA-A is a component of certain MHC class I cell surface receptor isoforms that resides on the surface of all nucleated cells and platelets. The receptor is a heterodimer, and is composed of a heavy, α chain, and smaller beta (β) chain. The alpha chain is encoded by a variant HLA-A gene and the beta chain (β2-microglobulin) is composed by the invariant Beta-2 microglobulin gene.
HLA A
MHC Class I molecules are part of a process that presents polypeptides from host of foreign derivation to the immune system. Normally if a peptide of foreign, pathogenic, source is detected it alerts the immune system that the cell may be infected with a virus, and thus target the cell for destruction.
For humans, as in most mammalian populations, MHC Class I molecules are extremely variable in their primary structure, and HLA-A is ranked among the genes in humans with the fastest evolving coding sequence. After typing millions of individuals, hundreds of variant alleles and isoforms have been identified.[1] This level of variation on MHC Class I is the primary cause of transplant rejection, as random transplantation between donor and host is unlikely to result in a matching of HLA-A, B or C antigens.
HLA-A gene
The HLA-A gene is part of the Human MHC complex on chromosome 6. The region is at the telomeric end of the HLA complex between the HLA-G and HLA-E genes. HLA-A gene encodes the larger, α-chain, constituent of HLA-A. Variation of HLA-A α-chain in certain ways is key to HLA function. This variation promotes diversity of class I recognition in the individual and also promotes genetic diversity in the population. This diversity allows more types of foreign, virus or cancer, antigens to be 'presented' on the cell surface, but also allows a subset of the population to survive if a new virus spreads rapidly through the population.
These changes are also key to inter-individual histocompatibility of organs and tissues. Difference in exposed structures of homologous proteins between individuals gives rise to antigen-antibody reactions when tissues are transplanted. This form of antigenicity gives rise to serotypes in tissue recipients. Refined serotypes are what scientist have used for grouping HLA.

ajor histocompatibility complex, class I, A,PDB rendering based on 1a1m.
There are a large number of variant alleles of the gene. The HLA-A gene was discovered after a long process of determining MHC antigens. The original alleles discovered for MHC class I were not separated according to genes. The first 15 HL A1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 contained antigens from many HLA loci. HL A1, 2, 3, 9, 10, 11 were later found limited to a maximum of 2 in any given person. For example, a person could have A1, A2, A7, A8 but not A1, A2, A3 and A11 or A7, A8, A14, A15. Given the exclusion HLA-A alleles were sorted according A and B, creating HLA-A and HLA-B serotype groups, in late 1970s the first A and B isoforms were finally sequenced
Alleles
There are a large number of alleles, so that classification by serotype simplifies categorization. For example HLA-A*0101, *0102, *0103, . . . *0130 are assigned to the serotype A1.The A*01 prefix signifies that the gene products (expressed proteins) of the alleles are primarily identified by the A1 serotype or most similar to alleles recognized by the serotype. There is a useful logic in this classification, HLA alleles evolve by a process called 'gene conversion' in which a few (<50 nucleotides) are swapped between HLA haplotypes and often results in the change of 1 to 3 nucleotides on the converted chromosome. Infrequently there are recombination events that cross-over a gene in the style of recombination we are familiar with in genetics. This can result in entirely new serotypes and alleles. Less frequently single nucleotide polymorphisms alters the gene (intro or exon) but can cause changes unseen at the protein level. These cryptic alleles are designated with further extension such as A*01010101 or A*01010102, but they are still A*0101 allele, also.
There are 673 gene alleles capable of producing 527 HLA-A isoforms and 46 nulls
HLA-A1
HLA-A1
HLA-A1 (A1) is a human leukocyte antigen serotype within HLA-A "A" serotype group. The serotype is determined by the antibody recognition of α1 subset of HLA-A α-chains. For A1, the alpha "A" chain are encoded by the HLA-A*01 allele group and the β-chain are encoded by B2M locus. This group currently is dominated by A*0101. A1 and A*01 are almost synonymous in meaning. A1 is more common in Europe than elsewhere, it is part of a long haplotype that appears to have been frequent in the ancient peoples of Northwestern Europe. A1 is a frequent component of the AH8.1 haplotype.
A1 serotype positivity is roughly linked to a large number of inflammatory diseases and conditions believed to have immune system involvement. Because of its linkage within the AH8.1 haplotype many studies showed association with A1 or A1,B8 only later to show the association drift toward the class II region gene alleles, DR3 and DQ2.5. While it is not clear what role A1 has in infectious disease, some linkage with infection rates in HIV remain associated within the A1 region of the haplotype.
A1 and autoimmune diseases
A1 serotype was associated with a number of diseases as "HL-A"' antigens were first being described. The associations rapidly expanded to include 'HL-A8' HLA-B8, as the HLA A1 and B8 were found to be commonly linked. As DRw3 was characterized, autoimmune risk drifted toward the class II region.
A1-B58 haplotype (A1-B17 where B58 is dominant) may remain associated with antineutrophil cytoplasmic antibodies (ANCA)
A1 in diabetes
With the exception of type 1 diabetes, most of the evidence for direct association of A1 with autoimmune diseases evaporated as DR3 and DQ2 genes were characterized. While type 1 diabetes shows an extended association on the HLA A1-B8-DR3-DQ2 haplotype, the association appears not to extend beyond the HLA-B locus.A recent study of DR3-DQ2/DR4-DQ8 phenotype found that A1-cw7-B8 was actually lower than expected relative to other A-B types, indicating that risk associated genes are located between B8 and DR3. However a study elsewhere showed that A*0101 appears to alter risk for type 1 diabetes but not Cw7-B8. The type 1 diabetes example shows the inherent difficulty in the use of linkage analysis alone to cipher risk.
A1 and allergic disease, sensitivities
Early in the study of HLA an association was found between HL A1,B8 in allergic disease, these are found to link to extended HLA A1-B8 region.
Oddly, A1 was also found associated with methotrexate-induced liver cirrhosis.Whereas A1 was found negatively associated with other disease such as coal workers pneumoconiosis and leprosy.
A1 and infectious disease
Within the early studies, A1 was found associate with or protected against some infectious diseases. Some diseases found associated with A1 actually link to the extended A1-B8 haplotype, viral induced hepatitis and accelerated progression of HIV are examples.
Further information: Infectious disease and A1-B8 haplotype
A1 with B8 showed an increase risk of measles infection, however, the significance was not consistent.A more recent paper showed an association of A*0101 with lower than average responses to measles vaccine.With rubella, A1-B8 was more frequently found in people infected as a result of maternal transefance.[16] A1 was also found to associate with circumoral herpes.[10] An association between A1 and cold sores was also described.
A1 in Lymphoma
In Hodgkin's lymphoma HLA-A1 but DR3 was not found higher. The A1-B8-DR3-DQ2 haplotype has a known association with Enteropathy-associated T-cell lymphoma, approximately 70% of patients are homozygotes for DQ2 with at least one copy of DR3-DQ2.
HLA-A2
HLA-A2 (A2) is a human leukocyte antigen serotype within HLA-A "A" serotype group. The serotype is determined by the antibody recognition of α2 subset of HLA-A α-chains. For A2, the alpha "A" chain are encoded by the HLA-A*02 allele group and the β-chain are encoded by B2M locus. A2 and A*02 are almost synonymous in meaning. A2 is more common in Northern Asia and North America than elsewhere, and it is part of a several long haplotypes.
The serotype identifies the gene products of many HLA-A*02 alleles, including HLA-A*0201, *0202, *0203, *0206, and *0207 gene products. A*02 is globally common, but A*0201 is at high frequencies in Northern Asia and North America. A2 is the most diverse serotype, showing diversity in Eastern Africa and Southwest Asia. While the frequency of A*0201 in Northern Asia is high, its diversity is limited to A*0201 the less common Asian variants A*0203, A*0206.

A2
Disease Associations
A2 Associated with spontaneous abortion in A2+/A[other] phenotypic children
HLA-A3
HLA-A3 (A3) is a human leukocyte antigen serotype within HLA-A serotype group. The serotype is determined by the antibody recognition of α3 subset of HLA-A α-chains. For A3, the alpha, "A", chain are encoded by the HLA-A*03 allele group and the β-chain are encoded by B2M locus. This group currently is dominated by A*0301. A3 and A*03 are almost synonymous in meaning.
A3 is more common in Western Eurasia, it is part of the longest known multigene haplotype, A3-B7-DR15-DQ6
Associated diseases
A3 serotype is a secondary risk factor for myasthenia gravis,lower CD8+ levels in hemochromatosis patients The HFE (Hemochromatosis) locus lies between A3 and B7 within the A3::DQ6 superhaplotype.[
In HIV
HLA-A3 selects HIV evolution for a mutation Gag KK9 epitope and results in a rapid decline in the CD8 T-cell response. CD8 T-cells are responsible for quickly killing HIV infected CD4+ cells.This type of evolved response may not be specific for HLA-A3 and since HIV is capable of adapting quickly in situ to selective factors.
HLA-A11
HLA-A11 (A11) is a human leukocyte antigen serotype within HLA-A "A" serotype group. The serotype is determined by the antibody recognition of α11 subset of HLA-A α-chains. For A11, the alpha "A" chain are encoded by the HLA-A*11 allele group and the β-chain are encoded by B2M locus. This group currently is dominated by A*1101. A11 and A*11 are almost synonymous in meaning.
In infectious disease
Associations have been observed between A11 and familial otosclerosis, pulmonary tuberculosis,leprosy,and cytomegalovirus infection with epilepsy. These and other studies suggest an involvement between A11 and secondary effects of certain herpes virus infections. A11 was also found increase in supraglottic cancer with poor 3 year survival.In osteosarcoma A11 was found elevated.
There is a strong association between anti-depressant induced hepatitis and HLA-A11. In autoimmune hepatitis, A11 has a synergistic effect, acting together with DR4 and DR3 to increase the odds of disease to over 300
A11 is also part of a haplotype A11-Cw4-B35-DR1-DQ1 that is a second factor in the rapid progression of HIV. The involvement of non-Hodgkin's lymphoma primaruily as a result of Epstein-Barr virus reinfection does not appear to be a cause in this acceleration.
Epstein-Barr Virus anomaly
There are at least a couple of forms of lymphoproliferative diseases that appear to arise from unresolved Epstein-Barr virus infection. Examination of the virus itself has led to the discovery of strains that can all but turn off the A11-mediated class I response to the virus in A11 enriched peoples (see tables below). This ability to turn off the immune system and for the virus to remain active is a factor in carcinogenesis. Early studies of A serotypes revealed and association of A11 with Hodgkin's lymphoma and recent studies have shown a complex involvement of Epstein-Barr virus infection as a consequence of low A11 control over infection.
Burkitt's lymphoma eventually lead to the discovery of the virus, however this disease is more evident in Africa. An involvement in cytotoxic T-lymphocytes down-regulation in Burkitt's lymphoma was subsequently discovered,More recent studies show A11 is down-regulated, and that other genetic defects are a likely cause.The ability to present EB virus antigens revealed a defect in the process after antigen process but before TAP1 involvement.Other studies indicated that peptides bind A11 in delivery to the cell surface for CTL screening, but fall off, and are destroyed intracellularly.However, A3 and A11 can process and load antigens even when proteosome activity is diminished suggesting an alternative mechanism for loading which may benefit in recovery from some disease but impair recovery of others.
It appears that these and other viruses have learned to exploit some defect in the region surrounding A11 that allows the near complete shut-down of gene expression. Oddly, in Africa A11 is at very low frequencies, and homozygotes are rare, suggesting that other genetic susceptibilities may exist that steer the virus toward Burkitt's lymphoma.
HLA-A36
HLA-A36 (A36) is a human leukocyte antigen serotype within HLA-A serotype group. The serotype is determined by the antibody recognition of α36 subset of HLA-A α-chains. For A36, the alpha "A" chain are encoded by the HLA-A*36 allele group and the β-chain are encoded by B2M locus. This group currently is dominated by A*3601. A36 and A*36 are almost synonymous in meaning.
A36 is more common in Africa (North and East) and Central Asia. A36 is rare HLA-A allele group.
Broad antigen
A 9
A 10
A 19
A 28
Split Antigens
A 23,24,25,26,34,43,66,29
HLA-B
HLA-B (major histocompatibility complex, class I, B) is a human gene that provides instructions for making a protein that plays a critical role in the immune system. HLA-B is part of a family of genes called the human leukocyte antigen (HLA) complex. The HLA complex helps the immune system distinguish the body's own proteins from proteins made by foreign invaders such as viruses and bacteria.
HLA is the human version of the major histocompatibility complex (MHC), a gene family that occurs in many species. Genes in this complex are separated into three basic groups: class I, class II, and class III. In humans, the HLA-B gene and two related genes, HLA-A and HLA-C, are the major genes in MHC class I.
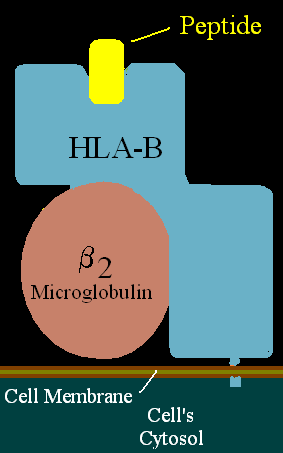
HLA B
MHC class I genes provide instructions for making proteins that are present on the surface of almost all cells. On the cell surface, these proteins are bound to protein fragments (peptides) that have been exported from within the cell. MHC class I proteins display these peptides to the immune system. If the immune system recognizes the peptides as foreign (such as viral or bacterial peptides), it responds by destroying the infected cell.
The HLA-B gene has many different normal variations, allowing each person's immune system to react to a wide range of foreign invaders. Hundreds of versions (alleles) of HLA-B are known, each of which is given a particular number (such as HLA-B27). Closely related alleles are categorized together; for example, at least 28 very similar alleles are subtypes of HLA-B27. These subtypes are designated as HLA-B*2701 to HLA-B*2728.
The HLA-B gene is located on the short (p) arm of chromosome 6 at position 21.3, from base pair 31,429,845 to base pair 31,432,923.
Ankylosing spondylitis: A version of the HLA-B gene called HLA-B27 increases the risk of developing ankylosing spondylitis. It is uncertain how HLA-B27 causes this increased risk. Researchers speculate that HLA-B27 may abnormally display to the immune system peptides that trigger arthritis. Other research suggests that joint inflammation characteristic of this disorder may result from improper folding of the HLA-B27 protein or the presence of abnormal forms of the protein on the cell surface. Although most patients with ankylosing spondylitis have the HLA-B27 variation, many people with this particular variation never develop the disorder. Other genetic and environmental factors are likely to affect the chances of developing ankylosing spondylitis and influence its progression.
HLA-B27 is associated with the spondyloarthropathies, a group of disorders that includes ankylosing spondylitis and other inflammatory joint diseases. Some of these diseases are associated with a common skin condition called psoriasis or chronic inflammatory bowel disorders (Crohn's disease and ulcerative colitis). One of the spondyloarthropathies, reactive arthritis, is typically triggered by bacterial infections of the gastrointestinal or genital tract. Following an infection, affected individuals may develop arthritis, back pain, and eye inflammation. Like ankylosing spondylitis, many factors probably contribute to the development of reactive arthritis and other spondyloarthropathies.
Other disorders: Several variations of the HLA-B gene are associated with adverse reactions to certain drugs. For example, two specific versions of this gene are related to increased drug sensitivity among the Han Chinese population. Individuals who have HLA-B*1502 are more likely to experience a severe skin disorder called Stevens-Johnson syndrome in response to carbamazepine (a drug used to treat seizures). Another version, HLA-B*5801, is associated with an increased risk of severe skin reactions in people treated with allopurinol (a drug used to treat gout, which is a form of arthritis caused by uric acid in the joints).
Among people with human immunodeficiency virus (HIV) infection, a version of HLA-B designated HLA-B*5701 is associated with an extreme sensitivity to abacavir. This drug is a treatment for HIV-1 that slows the spread of the virus in the body. People with abacavir hypersensitivity often develop a fever, chills, rash, upset stomach, and other symptoms when treated with this drug.
Several other variations of the HLA-B gene appear to play a role in the progression of HIV infection to acquired immunodeficiency syndrome (AIDS). AIDS is a disease that damages the immune system, preventing it from effectively defending the body against infections. The signs and symptoms of AIDS may not appear until 10 years or more after infection with HIV. Studies suggest that people with HIV infection who have HLA-B27 or HLA-B57 tend to progress more slowly than usual to AIDS. On the other hand, researchers believe that HIV-positive individuals who have HLA-B35 tend to develop the signs and symptoms of AIDS more quickly than usual. Other factors also influence the progression of HIV to AIDS.
Another version of the HLA-B gene, HLA-B53, has been shown to help protect against severe malaria . HLA-B53 is most common in West African populations, where malaria is a frequent cause of death in children. Researchers suggest that this version of the HLA-B gene may help the immune system respond more effectively to the parasite that causes malaria.
HLA-B SEROTYPES · B5 (B51 · B52) · B7 · B8 · B12 (B44 · B45) · B13 · B14 (B64 · B65) · B15 (B62 · B63 · B70 · B71 · B72 · B75 · B76 · B77) · B16 (B38 · B39) · B17 (B57 · B58) · B18 · B21 (B49 · B50) · B22 (B54 · B55 · B56) · B27 · B35 · B37 · B40 (B60 · B61) · B41 · B42 · B46 · B47 · B48 · B53 · B59 · B67 · B73 · B78 · B81 · B*82 · B*83
HLA-C
HLA-C belongs to the MHC (human = HLA) class I heavy chain receptors. The C receptor is a heterodimer consisting of a HLA-C mature gene product and β2-microglobulin. The mature C chain is anchored in the membrane. MHC Class I molecules, like HLA-C, are expressed in nearly all cells, and present small peptides to the immune system which surveys for non-self peptides.

HLA-C is a locus on chromosome 6 that encodes for a large number of HLA-C alleles that are Class-I MHC receptors. HLA-C is localized proximal to the HLA-B locus is located on the distal end of the HLA region. Most HLA Cw:B haplotypes are in strong linkage disequilibrium and many are as ancient as the human species itself.
Disease Associations
By Serotype
Cw1: Multinodular goiters
By Allele
Cw*16: B chronic lymphocytic leukemia
Nomenclature
Cw*01
* Cw1 Serotype: Cw*0102 and Cw*0109
* Cw11 ?
* Cw*0104 to *0108
Cw*02
* Cw2 Serotype: Cw*0202 and *0208
* Cw*0203 to *0207, and 0209
Cw*03
* Cw9 Serotype: Cw*0303
* Cw10 Serotype: Cw*0302, *0304, and *0306
* Cw3 Serotype: Cw*0307
* Cw*0305 and 0308
Cw*04
* Cw4 Serotype: Cw*0401, *0407, and *0410
Cw*05
* Cw5 Serotype: Cw*0501 and *0502
* Cw*0503 to *506 and *0508 to *0510
Cw*06
* Cw6 Serotype: Cw*0602 and *0605
* Cw6*0603, *0604 and *0606 to *0611
* Cw7 Serotype: Cw*0701 to *0706, *0712, *0714, *0716
* Cw*0707 to *0711, *0713, *0715, and *0717 to *0729
Cw*08
* Cw8 Serotype: Cw*0801, *0802 and *0803
* Cw*805 to *0812
Cw*1202 to *1215
Cw*1402 to *1405
Cw*1501 to *1511
Cw*1601 to *1606
Cw*1701 to *1703
Cw*1801 and *1802
Common Haplotype
Cw4-B35 (Western Africa to Native Americans) Cw7-B7 (Western Eurasia, South Africa) Cw7-B8 (Western Eurasia) Cw1-B46 (China, Indochina) Cw5-B44 (Western Eurasia)
Afyon
ReplyDeleteBalıkesir
Kırklareli
Amasya
Bilecik
4Q5NK
bitlis
ReplyDeletesakarya
van
tunceli
ankara
RPS
goruntulu show
ReplyDeleteücretli
78P6TU
sakarya evden eve nakliyat
ReplyDeleteosmaniye evden eve nakliyat
aksaray evden eve nakliyat
çanakkale evden eve nakliyat
zonguldak evden eve nakliyat
73D3Z
1193B
ReplyDeleteTekirdağ Lojistik
Gümüşhane Lojistik
Kırşehir Parça Eşya Taşıma
Sivas Evden Eve Nakliyat
Erzincan Evden Eve Nakliyat
89724
ReplyDeleteÇerkezköy Çelik Kapı
Çankaya Boya Ustası
Gümüşhane Parça Eşya Taşıma
Nevşehir Parça Eşya Taşıma
İstanbul Lojistik
Aydın Lojistik
Çanakkale Parça Eşya Taşıma
Burdur Şehir İçi Nakliyat
Bartın Lojistik
8E83D
ReplyDeletehttps://steroidsbuy.net/
Eskişehir Evden Eve Nakliyat
order sustanon
Manisa Evden Eve Nakliyat
order parabolan
buy sarms
pharmacy steroids for sale
Paribu Güvenilir mi
order oxandrolone anavar
61281
ReplyDeleteSiirt Evden Eve Nakliyat
Uşak Parça Eşya Taşıma
Omlira Coin Hangi Borsada
Tekirdağ Parça Eşya Taşıma
Ardahan Parça Eşya Taşıma
Antalya Lojistik
Ankara Evden Eve Nakliyat
Adana Şehirler Arası Nakliyat
Gate io Güvenilir mi
A758A
ReplyDeletePursaklar Boya Ustası
Tokat Evden Eve Nakliyat
Kırklareli Parça Eşya Taşıma
Omlira Coin Hangi Borsada
İstanbul Evden Eve Nakliyat
Hatay Şehirler Arası Nakliyat
Adana Evden Eve Nakliyat
Bitlis Evden Eve Nakliyat
Afyon Parça Eşya Taşıma
4FDDC
ReplyDeletewinstrol stanozolol
Sakarya Evden Eve Nakliyat
Bilecik Evden Eve Nakliyat
Karabük Evden Eve Nakliyat
Diyarbakır Evden Eve Nakliyat
turinabol for sale
for sale dianabol methandienone
Adıyaman Evden Eve Nakliyat
Kayseri Evden Eve Nakliyat
B793A
ReplyDeletehttps://referanskodunedir.com.tr/
8D2EE
ReplyDeletekırıkkale mobil sohbet odaları
çankırı goruntulu sohbet
bolu canli sohbet bedava
sohbet siteleri
kayseri mobil sohbet sitesi
balıkesir ücretsiz sohbet
kastamonu canlı sohbet odaları
edirne canli sohbet chat
random görüntülü sohbet
5584F
ReplyDeletebedava görüntülü sohbet sitesi
görüntülü sohbet siteleri ücretsiz
sivas ücretsiz görüntülü sohbet uygulamaları
canli sohbet bedava
adana telefonda rastgele sohbet
Kayseri Ücretsiz Sohbet Siteleri
rastgele sohbet
ağrı kadınlarla sohbet et
Çorum Parasız Sohbet
11DC5
ReplyDeleteeskişehir canlı görüntülü sohbet
canlı sohbet siteleri
artvin canlı görüntülü sohbet uygulamaları
chat sohbet
Tokat Görüntülü Sohbet
Rize Mobil Sesli Sohbet
Konya Sohbet Muhabbet
kadınlarla sohbet
kırşehir canlı sohbet et
B795E
ReplyDeleteThreads Beğeni Satın Al
Referans Kimliği Nedir
Lovely Coin Hangi Borsada
Binance Referans Kodu
Telegram Görüntüleme Satın Al
Youtube Beğeni Satın Al
Apenft Coin Hangi Borsada
Azero Coin Hangi Borsada
Bitcoin Yatırımı Nasıl Yapılır
CBDF0
ReplyDeleteSui Coin Hangi Borsada
Kwai Takipçi Satın Al
Bulut Madenciliği Nedir
Gate io Borsası Güvenilir mi
Görüntülü Sohbet Parasız
Meta Coin Hangi Borsada
Threads Takipçi Satın Al
Ön Satış Coin Nasıl Alınır
Coin Kazma Siteleri
AFFAC93B15
ReplyDeletegerçek takipçi satın al
899B211B2B
ReplyDeletetakipçi fiyat
06E7CBAF5F
ReplyDeletetakipçi al
94283069C0
ReplyDeleteinstagram kadın takipçi
شركة تركيب طارد الحمام بالنعيرية LloWoYDZlx
ReplyDeleteشركة كشف تسربات المياه بالدمام dr8UBE8jrq
ReplyDeleteشركة كشف تسربات المياه بالدمام huPBQea6wV
ReplyDelete8EA9196599
ReplyDeleteTelegram Farm Botları
Telegram Para Kazanma Botları
Telegram Coin Botları
Telegram Para Kazanma
Binance Hesabı
شركة نقل عفش بالكويت
ReplyDeletePrjST9avsX2r3